Travelling with diabetes means there are a few more things to think about before you set off. But living with diabetes shouldn't be a barrier to taking trips or holidays at home or abroad.
Plan to take two to three times the amount of insulin or other diabetes medication and equipment you’d normally use. This will give you peace of mind if you have to stay longer for any reason or if there are disruptions.
If you’re travelling abroad, a little extra planning can go a long way to help you relax and enjoy yourself. Don't forget your doctor's letter and travel insurance.
Use our tips below to skip to other information you need.
- Organise medication with your healthcare team
- What to pack in your hand luggage.
- Flying with a CGM, insulin pump or Freestyle Libre
- Crossing time zones
- Looking after diabetes in hot climates
- Looking after diabetes in cold climates
Checklist for people travelling with diabetes
Check your airline’s guidelines for people with diabetes
Contact your airline or other operator or look on their website for their guidelines for people living with diabetes. You may need to complete forms in advance, particularly if you use an insulin pump or continuous glucose monitor (CGM). You can also check health information for the country you’re visiting – follow the links on the Foreign travel advice page on the gov.uk website.
Organise medication with your healthcare team
Get extra supplies of medication, device spares, and backup
Ask your healthcare team for prescriptions for extra insulin, other diabetes medication, and if you use devices, extra supplies and manual equipment. Flying with an insulin pump, CGM or Freestyle Libre shouldn’t be a problem. But it is sensible to have back up in case of a failure. Expect to take two to three times the amount of medication or supplies you'd usually need.
Get advice on adjusting insulin on long-haul flights
If you are going on a long-haul flight discuss this with your healthcare team. They will advise on any adjustments to your insulin injections or insulin pump - or medication that may be required if you are crossing time zones.
Request a travel letter about your diabetes
In some cases, you may be required to get a letter from your healthcare team stating you have diabetes and that you need to carry medical supplies. The letter should include details about your medication, if for any reason you need to carry medication in containers over 100mls, and any devices that you use.
Please check with the airline before you travel as a letter may be requested by some airlines and other operators and is helpful in the event of an emergency.
It is also advisable to take a copy of a recent prescription with you in case you should need to get supplies whilst away. If you have the NHS app on your mobile phone this also shows your GP record and repeat prescription information.
Download a medical awareness card
If you use a CGM, insulin pump, or Freestyle Libre, and are flying, download a Medical Device Awareness Card (PDF, 71KB) from the City Aviation Authority's website to go with your doctor's letter. The card is not essential, but it may make things easier. You show this to airport security officers with your letter, as it sets out the rules on screening if you wear a medical device.
Check insulin supply in the destination country
Before travelling, find out where you can get supplies of insulin at your destination in case of emergency. Contact your insulin manufacturer before the trip to see if your insulin is supplied in the country you are travelling to.
Insulin manufacturers - contact details
| Manufacturer | Contact number |
| Eli Lilly & Company | 01256 315000 |
| Novo Nordisk Ltd | 0800 0232 573 |
| Sanofi | 0800 035 2525 |
| Wockhardt UK | 01978 661261 |
Managing insulin when crossing time zones
Long-haul flights east or west involve crossing time zones. And you may need to adjust your insulin. Eastward travel will shorten the day, and generally mean a temporary reduction in insulin doses, whereas westward travel will extend the day, and possibly increase insulin requirements.
Speak to your healthcare team for advice about adjusting your insulin doses. Have your flight details to hand including your departure time, the length of the flight, and the local time of arrival.
Time zones and tablets
If you take diabetes tablets, you are unlikely to have any particular problems. Very occasionally, it may be necessary to take extra tablets to cover a longer day. Do discuss this with your diabetes care team beforehand.
You may, on occasions, need to leave out one dose of tablets on a short day, when you are travelling on a long west to east journey. Speak to your diabetes care team about this well in advance of the trip.
Crossing time zones and using an insulin pump, CGM or Freestyle Libre
If you are going on a long-haul flight, you may cross different time zones.
When crossing different time zones, you may need to change the time or date on some insulin pumps manually so you get the correct basal insulin dose. Speak with your healthcare provider before you travel to get their advice on which settings to change and when.
If you use an app, the date and time on smartphones should automatically update when travelling across time zones. If you use a Freestyle Libre reader, you will manually need to adjust the time for accurate reports.
Storing insulin
If you're travelling somewhere hot, remember that heat can damage your insulin and stop it from working properly. Insulin damaged by heat may have a brownish colour, and clear insulin may become cloudy. Do not use insulin that looks like this.
When travelling with insulin, it is best to keep it cool by storing it in a hotel fridge (if there is one in your room) or in a cool bag (providing it does not freeze). A variety of cool bags and storage containers are available. If using a cool bag that uses plastic ice blocks, make sure that the insulin does not come into contact with the frozen plastic containers.
Get more information on managing diabetes in hot weather.
Storing insulin in cold climates
Insulin can freeze in very extreme temperatures but cannot be used if it has been frozen, so if you are planning to visit the arctic (or somewhere equally cold) make sure you keep insulin at room temperature or even on you in an inside pocket or pouch close to your body, to ensure it doesn’t freeze.
Get more information on managing diabetes in cold weather.
Get travel insurance
If you have diabetes, travel insurance is important. You want peace of mind that any emergency medical costs for your diabetes or any other medical condition is covered.
Make sure that any travel insurance covers pre-existing medical conditions like diabetes, as many don’t. It’s also really important you ask if they cover coronavirus in case you need treatment while you’re away.
You can also check health information for the country you’re visiting – see the Foreign travel advice page on the gov.uk website.
UK residents travelling to the EU still have access to emergency and necessary healthcare. (See the guidance on travelling with an existing medical condition if you go to the EU).
However, we still advise that you get travel insurance because free health cover provided by the European Health Insurance Card (EHIC) and Global Health Insurance Card (GHIC) doesn’t cover certain things like emergency repatriation (if you need to come home) and not all countries give the same level of cover as the NHS.
If you have diabetes and planning a trip, we can help you get coronavirus-covered travel insurance with AllClear Insure My Diabetes.
What to pack in your hand luggage
- All diabetes medication
- Diabetes supplies – including sensors and other device spares
- Diabetes identity card or wrist band
- A letter from your doctor about your diabetes and treatment and if you use an insulin pump, CGM or flash glucose monitor.
- A prescription sheet
- Hypo treatments
- Extra snacks in case of delays like nuts, fruit or a sandwich.
Split meds between separate bags if you can, for example, if you’re travelling with a partner or friend, in case you lose something.
"Be prepared. I always travel with a backpack full of snacks, medication and everything I need. I don't rely on airport shops being open or other amenities. And when I'm in the mountains, I always have at least three snacks with me." Read Lee's story.
Can I carry insulin in my hand luggage?
Always carry insulin, other diabetes medication, device spares, hypo treatments and other diabetes supplies in hand luggage. It’s important to keep insulin in hand luggage as being in the hold can damage it as it’s so cold and luggage can be lost.
Sensors or other device spares must go in hand luggage as they can be damaged by hold luggage X-rays.
Medication restrictions at the airport
Carrying a doctor’s letter from your GP is requested by some airlines and is helpful to show airport security if there is any confusion.
Current security regulations state that liquid items are only allowed in your hand luggage if they are in containers 100mls or less. There is no restriction on the number of tablets you can take through airport security but they should be mentioned in your doctor’s letter.
Flying with an insulin pump, CGM or Freestyle Libre
It's sensible to look up the manufacturer's advice on flying with your particular device.
Insulin pumps are safe for use during air travel and you can continue to use CGM or flash glucose sensors whilst flying. Connect them to the handset or your phone using Bluetooth. They will still work if your phone is on airplane mode.
If you use an insulin pump, be aware that changes in air pressure when flying can change the amount of insulin delivered by the insulin pump. So it is important to monitor your blood sugar levels more closely on flights, especially around take-off and landing.
When you buy your ticket, contact your airline or other operator or look on their website for their guidelines for people living with diabetes. You may need to complete forms in advance, particularly if you use an insulin pump or continuous glucose monitor (CGM). If you don't do this, in some cases it may cause delay.
If you use a CGM, insulin pump or Freestyle Libre, security staff may ask to see evidence that you need to use one – so you’ll need a letter from your GP or healthcare team to say so.
You can also print off a Medical Device Awareness Card (PDF, 71KB) from the Civil Aviation Authority website to go with your letter. This sets out screening advice for you (the passenger) and the security officer carrying out the checks.
You should also speak to your diabetes team before you go. They can give your more advice about travelling with diabetes on planes. And should you need to remove your pump for any reason, they can provide you with any extra equipment like insulin pens and help plan your doses throughout your journey.
"Since I've been using the Dexcom CGM I’ve been surfing, I’ve been on solo holidays, I’ve been abroad. I’ve done all the things I wasn’t sure I’d be able to do when I first got diagnosed." Georgia.
Can CGMs, insulin pumps and Freestyle Libre sensors go through airport security scanners?
Not all diabetes technology can safely go through security checks at airports. It's important to speak with your healthcare team and look up the manufacturer's security scanning advice for your particular device. We have general guidance below.
Guidance on metal detectors and CGMs and pumps
Most types of CGM/Freestyle Libre sensors and insulin pumps can be taken through the metal detector arches that you walk through.
X-ray luggage scanners, body scanners and CGMS and pumps
Most types of CGM/Freestyle Libre sensors and insulin pumps - and any spare devices or sensors - should not be exposed to x-ray luggage scanners, hold luggage scanners or full body scanners.
If you don’t want to remove your CGM/sensor/insulin pump to go through a full body scanner, ask for a “pat down” instead. Please be aware that this may take some time, as a pat down might need to be completed by a specific member of staff, so it may be helpful to factor this into your travel plans and leave plenty of time to go through airport security.
You should never be asked to remove a medical device from your body for screening. And you should be offered alternative methods of screening.
Carrying a Medical Device awareness card (PDF, 71KB) along with your GP’s letter reminds you and the security staff of the screening advice for medical devices.
What to eat on the plane
Airlines can provide information on the times of most meals so you can plan your insulin.
It is best to order the standard meal, though this may not supply you with enough carbohydrates if you are on insulin or certain diabetes tablets. Cabin crew are usually able to provide fruit, crackers or rolls.
On long flights, you may need snacks in between meals and at bedtime to prevent blood sugar levels going too low. If you use insulin, monitor your blood sugar levels frequently and be prepared to make changes to your dosage.
Looking after diabetes in hot climates
In hot countries, the biggest health threat is the sun, so keep covered.
Wear clothes that cover and protect your skin and make sure you wear high factor sunscreen. People often miss the backs of their hands and necks, so make sure you keep these covered and protected with sunscreen.
Sunglasses should also have a UV400 label to make sure they protect your eyes.
Take particular care of your feet if you have neuropathy which is numbness in your feet. This can mean you’re not aware skin is burning so protect them from the sun with socks or sunscreen. Make sure you wear well-fitting sandals on the beach, so they don’t burn on the hot sand.
Sunbathing and blood sugar levels
Sunbathing on the beach can make your blood sugar levels higher than normal because you're not being very active.
Your insulin may be absorbed more quickly from the injection site in hot weather too, and this increases the risk of hypos. You’ll need to monitor your levels more often and be ready to adjust your diet or insulin dose.
Be careful of misleading test results because the extremes of temperature may affect the accuracy of your blood glucose meter.
Find out more about diabetes and hot weather.
Looking after diabetes in cold weather and climates
In cold weather, your insulin may be absorbed more slowly at first, but can then be absorbed suddenly when you warm up later in the day. This can cause you to have a hypo. If your body also uses up more energy staying warm, for example shivering, this can lead to hypos too. So it can be useful to wear layers in colder climates which will both help to keep you warm and allow you to remove clothing if you need to as you warm up.
Hypos are more dangerous in cold conditions. This is because they interfere with your body’s attempts to stay warm and increase the risk of hypothermia. So you may need to monitor your levels more often and be ready to adjust your diet or insulin dose if needed.
Guarding against hypos is really important so remember your meter may not be accurate in cold conditions. If you are heading somewhere with extreme cold weather check the meter instructions for temperatures it will be accurate at and keep it wherever possible at room temperature.
If you suffer from poor circulation or have neuropathy, it's particularly important to prevent frostbite, because the numbness in your feet can mean you don't feel the cold. Make sure you check your feet regularly in cold countries and take plenty of layers including spare socks.
Find out more about storing insulin.
Keeping to your diabetes routines when you're away
It’s important to remember your routines for managing diabetes when you’re abroad. Your job isn’t to avoid trying new things or enjoying yourself. It’s just to be aware that eating different foods, becoming more or less active or drinking alcohol can all make a difference to your blood sugar levels. So check regularly and keep yourself safe.
“As well as a letter from my GP, my phone comes with a health app that I’ve put information about my diabetes and medication in. In an emergency, people can access this without having to unlock my phone.” Lucy.
If you have a tummy bug or you find yourself unable to eat or drink, follow your sick day rules. If you develop covid symptoms while abroad or during travel, you must review the local regulations and follow local public health guidance if available.
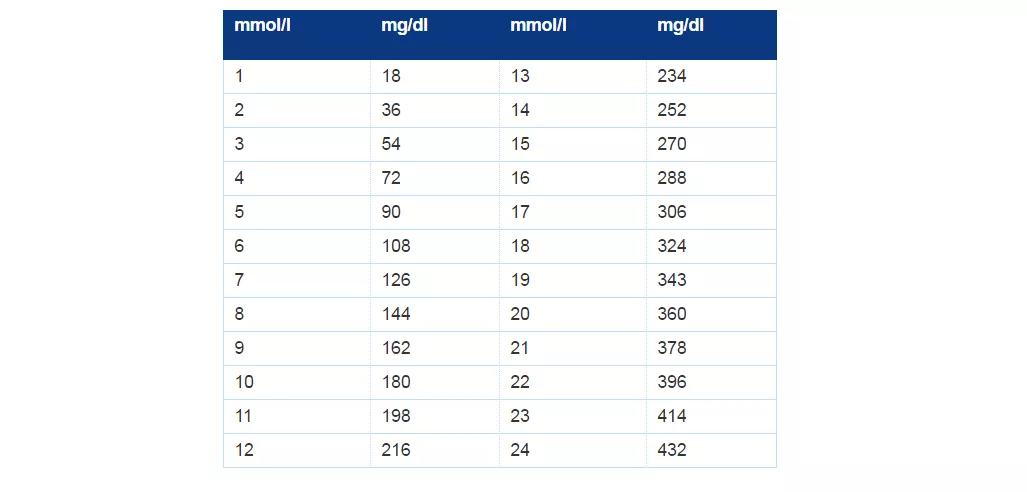
If the worst comes to the worst and you find you need to go to the hospital while away, don't be alarmed if your blood sugar levels are described differently. Some countries measure blood sugar in milligrams per decileter instead of millimoles per litre - take a look at our blood glucose conversion chart below.