Gareth and Joanne
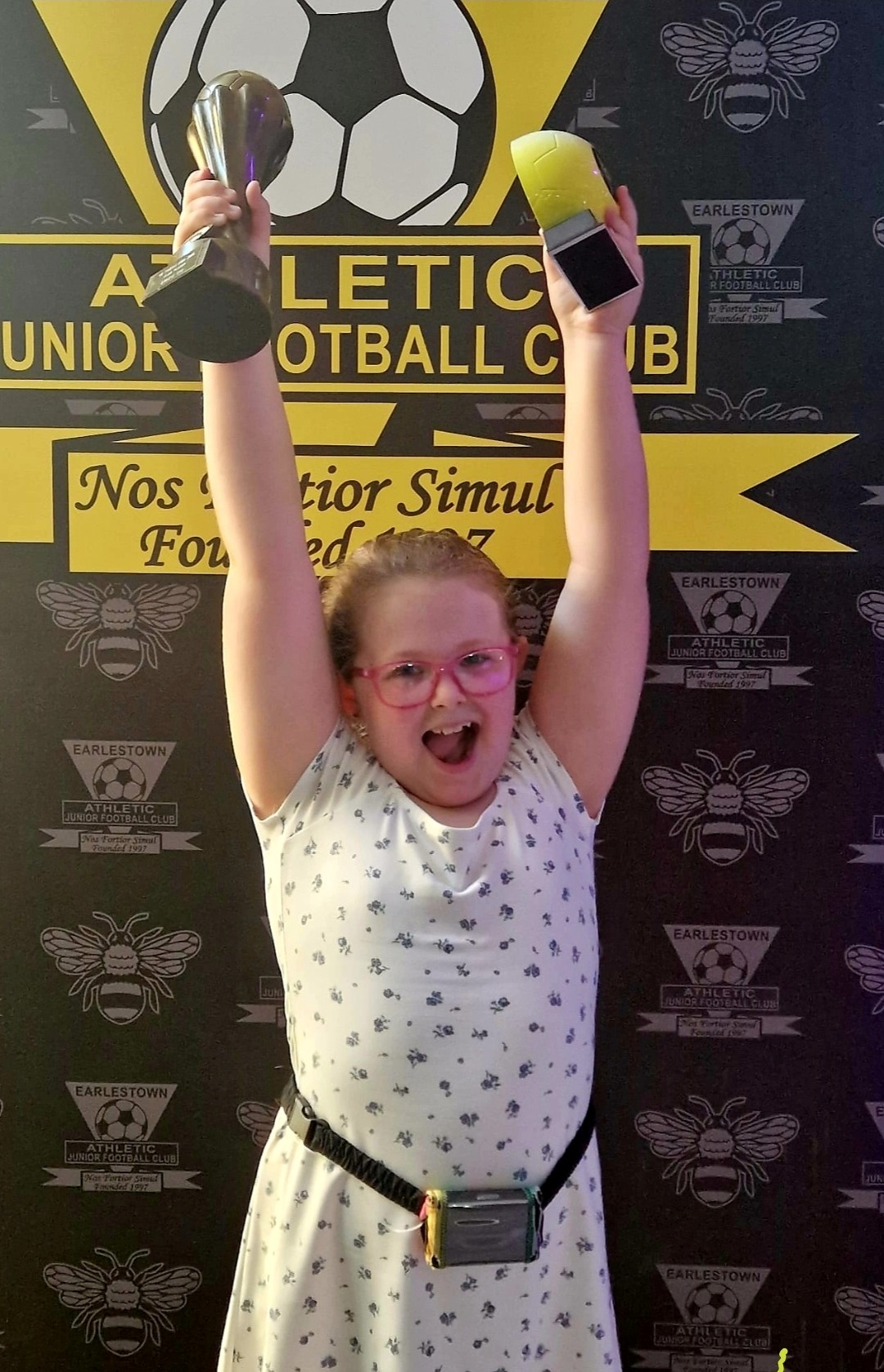
Whether or not a cure comes in her lifetime, we know it’ll be okay because she’s already proving that diabetes doesn’t define her.
Gareth and Joanne Nye live in Newton-le-Willows along with their three children. In November 2018, when their daughter Gracie was rushed to hospital with diabetic ketoacidosis (DKA), their world changed overnight. Here, they share their experience of Gracie being diagnosed with type 1 diabetes – and how it has shaped family life since.