Tackling Inequity Strategy
Our Tackling Inequity Strategy sets out our vision and plans to tackle unfairness in diabetes care, and to ensure everyone — no matter their background, identity or circumstances — can access the treatment, support and opportunities they need to live well.
Our strategy is built on the insights, experiences and priorities of people living with or at risk of diabetes and is shaped in partnership with communities, healthcare professionals and organisations across the UK.
Read our full strategy here, No One Left Behind - Achieving equity in diabetes: 2025-2030 Strategy (PDF, 6,247KB), or you can read the strategy in full below.

We are deeply grateful to the following organisations whose expertise, commitment, and shared drive to achieve equity for everyone at risk of or affected by diabetes have helped shape this strategy. Their insights have been invaluable in ensuring this document reflects the diverse needs and experiences of our communities.
No One Left Behind
Achieving equity in diabetes: 2025-2030 strategy
Tackling inequity is a top priority for Diabetes UK, and this strategy unites our internal efforts on Equity, Diversity, and Inclusion with actions to challenge systemic inequalities.
You can take a look at the full strategy below, or alternatively you can use the links below to navigate to different sections of the strategy - from our shared vision to the priority actions we’re taking over the next five years and how we’ll hold ourselves to account.
- A shared vision for equity
- Our five-year priority actions
- Holding ourselves to account
- The story of this strategy
A shared vision for equity
Developed from the insights, hopes and priorities of people living with or at risk of diabetes, and those who work with them—this is the UK we all want to see.
In a world where diabetes can do no harm and no one is left behind:
- Research is representative of the diabetes population, so that discoveries benefit everyone by shaping tailored and appropriate care.
- Services and environments for people living with or at risk of diabetes are antiracist, poverty-aware, disability-aware and trauma-informed.
- Diabetes is free from stigma, with resources and support allocated and delivered without blame or judgement.
- New tests, treatments and technologies are rolled out with sustainable and proactive plans to monitor and address any inequity including geographical variation or accessibility adjustments.
- Type 2 diabetes screening programmes are focused on those at highest risk, with adjusted thresholds for those who need it most.
- National policies support access to affordable healthy foods, green spaces, secure housing and good working conditions, recognising the role of these in the ability to self-manage all types of diabetes and in the prevention of type 2.
No matter our background, identity, ability or circumstances, everyone living with diabetes can access:
- Timely and supportive diagnosis, following early recognition of risk.
- Prevention and remission support which is culturally relevant, tailored to specific needs and which addresses barriers to engagement.
- Regular diabetes check-ups, delivered by an appropriately trained provider.
- Diabetes dietary advice, recommended treatments and technology, with appropriate accessibility adjustments for people living with physical disabilities.
- Person-centred, tailored and coordinated care to enable effective self-management of diabetes throughout life, including where it coexists with other long-term conditions, and adapted for disability or additional needs.
- High quality diabetes information delivered to take account of access needs, including translation or easy read materials as well as adjustments for visual or hearing impairment.
- Diabetes-informed inpatient hospital care that protects safe and effective diabetes management.
- Comprehensive support for sex-specific health needs including sexual health, pregnancy, menstrual health and menopause in diabetes.
- Emotional and mental health support, which recognises the emotional toll a diabetes diagnosis can take as well as the additional challenges of self-managing diabetes whilst living with a severe mental illness.
Our five-year priority actions
The four Cs
These principles were developed during the 2023 Tackling Inequality Commission to frame their thinking and guide their approach. The four Cs continue to underpin everything we do.

Context – we will consider the different and intersectional factors that result in inequity. We will adapt our work to remove barriers, recognise where we may be creating unnecessary barriers and direct resources to where there is greatest need.

Curiosity – we will listen and learn, remain open to challenge and proactively seek involvement and critical feedback from people with lived experience, trusted leaders in underserved communities and other experts.

Collaboration – we will work in equal partnership with individuals living with diabetes, community leaders and organisations who support those who face inequity. We recognise that we won’t always be the organisation to lead, but may add value by lending our voice and support.

Commitment – we will show leadership in this area, confront difficult conversations and advocate boldly for people who face inequity. We will demonstrate our accountability through yearly impact reporting.
1. Improve our support for communities affected by diabetes inequities.
We will:
- Be a loud and influential voice that amplifies and champions communities experiencing diabetes inequity, including challenging narratives that perpetuate stigma or stereotypes around diabetes and ethnicity, socio-economic background, disability and obesity.
- Work to build trust in underserved communities through transparency, representation, advocacy and equal partnership, starting with our Community Organisation Advisory Committee.
- Make all of our information and support services relevant, inclusive and accessible.
- Tailor information and support to meet the needs of people with diabetes who also manage multiple long-term conditions or diabetes complications.
- Improve our overall reach, aiming for it to reflect the diabetes population.
- Provide inclusive and non-judgmental helpline support, through staff training and policies that are antiracist, culturally competent, poverty- and disability- aware and trauma-informed.
- Achieve representative uptake of our learning zone online self-management platform through targeted community-based promotion.
2. Build the evidence base around diabetes inequities and ensure diabetes research benefits all.
We will:
- Use annual highlight notices to ringfence a proportion of our research investment into reducing healthcare inequities.
- Ensure our research funding processes are inclusive, fair, and transparent so that Diabetes UK-funded researchers reflect the diverse populations of the UK
- Inspire and enable researchers of all backgrounds to work in diabetes so that by 2030 we have 10 times more research staff from Black backgrounds funded through Diabetes UK.
- Require researchers to embed equity into all funding applications, through policies such as inclusive study design, diverse and representative participation, and analysis of disaggregated data.
- Ensure that, where appropriate, all Diabetes UK funded research includes a clear plan for how it will be implemented within specific communities, highlighting the value of diverse participation. Implementation strategies should be tailored to meet the unique needs of different groups and co-designed with those directly affected, to maximise real-world relevance, effectiveness, and impact.
- Collaborate with community organisations and stakeholders to identify pressing research questions related to underserved communications, so that 20% of our funding is directed to these issues by 2030.
- Influence to achieve systematic collection and analysis of data to improve insight into poorly understood areas of diabetes inequity, as highlighted by Core20PLUS5. For instance, around people with intellectual and physical disabilities, homelessness and vulnerable migrants.
See our Diabetes UK Research Strategy for our detailed plans.
3. Advocate for equitable change with or for people with or at risk of diabetes.
We will:
- Communicate the seriousness of diabetes, and campaign to ensure it remains a political priority.
- Campaign for governments to address diabetes inequities through public health policy, health service reforms, tackling poverty and creating healthier food environments.
- Position diabetes as a cornerstone inequity among policymakers—a fundamental issue that is central to tackling wider UK health inequities.
- Challenge diabetes stigma wherever it appears by working to improve public understanding of its complexity and realities.
- Be an active partner in campaigns that push government to act on poverty and the food environment.
4. Drive equitable diabetes healthcare.
We will:
- Adopt and promote the NHS Race & Health Observatory’s Seven Anti-Racism Principles among health systems.
- Support and influence national and local health systems to identify challenges, implement solutions, and ensure accountability in the equitable delivery of safe, accessible and coordinated care, delivered by appropriately trained staff. In particular:
- Early and supportive diagnosis, including signposting to our resources for 125,000 newly diagnosed individuals every year.
- Early identification of pre-diabetes, plus prevention and remission support for type 2 diabetes, particularly for those under 40.
- Prevention support for women with gestational diabetes, aiming to roll out our awareness raising ‘traffic light’ tool for women across the UK by the end of 2026
- All recommended diabetes care processes, achieving year-on-year increases and reaching for 90% equitable uptake by 2030.
- Ensuring new treatments and technologies are equitably available to all who could benefit.
- Women’s health services, including sexual health and contraception, pregnancy, menstrual health and menopause in diabetes.
- Highlight to health systems the needs of vulnerable groups, including those with people living with disabilities, multiple long-term conditions, severe mental illness, or experiencing homelessness or institutional care.
- Ensure that diabetes healthcare professionals can access cultural and disability competency training so that they understand and are aware of their role in addressing diabetes health inequity and have the tools to do so.
5. Grow as a diverse and inclusive organisation.
We will:
- Embed antiracism, poverty and disability awareness in Diabetes UK culture, ways of working, systems and processes, aiming for 90% of colleagues saying ‘People of all cultures and backgrounds are respected within Diabetes UK’ in the 2030 pulse survey.
- Attract, retain and grow diverse talent at all levels of our organisation so that we reflect the communities we serve and build a pipeline for future leadership within Diabetes UK and the broader charity sector.
- Attract volunteers from diverse backgrounds, aiming for yearly increases across demographic groups so that our volunteer population represents the communities we serve.
- Make volunteering accessible. Remove barriers to joining Diabetes UK as a volunteer and diversify the ways people can get involved.
- Equip volunteers to support our equity aims by providing antiracism, poverty, disability and stigma awareness training.
- Diversify all Diabetes UK committees and panels to ensure they reflect the ethnicity and socioeconomic diversity of the UK diabetes population.
- Equip staff and volunteers with the knowledge, skills and behaviours to work with the communities we serve.
- Work only with suppliers who demonstrate a strong commitment to EDI.
See our Equity, Diversity and Inclusion 5-Year Action Plan: Colleagues and Volunteers (PDF, 1,539KB) for our detailed plans.
Holding ourselves to account
Tackling diabetes inequity is a collaborative endeavour, so being open about our progress and the lessons we learn along the way is essential to achieving our collective goals.
We’re committed to reporting on our milestones, successes and failures, and being held to account by our Board, our supporters and the wider diabetes community. We will also work with, and seek advice from ‘critical friends’, such as the NHS Race and Health Observatory.
We will:
- Publish our detailed EDI plans for the charity and for our research programme, setting out clear targets and milestones.
- Report progress in all areas against our action plans for equity in our Annual Report and Accounts.
- Publish insights and feedback from our Diabetes Lived Experience Advisory Committee and Community Organisation Advisory Committee along with the actions we have taken in response.
The story of this strategy
Unfairness in diabetes has long existed but has been exacerbated by the effects of austerity and the Covid-19 pandemic.
We have put increasing focus on these issues in recent years. Now we are positioned to become a key facilitator in reducing the root causes of disparities in diabetes and to lead the way towards health equity and better outcomes for all.
The foundations
The Diabetes UK 2020-2025 charity strategy [i] identified ‘Addressing and Fighting Inequality’ as one of four cross-cutting themes needed to drive progress towards our mission.
Since then, we have worked with people living with diabetes, frontline healthcare workers, researchers and policy experts to help us become more inclusive as a charity and influence change across governments, health systems and diabetes services.
In 2022, our ‘health inequalities in diabetes workshop’ brought together research experts, healthcare professionals and people living with diabetes to define key research priorities in this area [ii]. And in 2023, our Tackling Inequality Commission amplified diverse voices of people with diabetes and issued a clear call for systemic change [iii].
A shared vision
The development of this strategy—No One Left Behind. Achieving equity in diabetes: 2025-2030 strategy—has been built on these foundations and shaped by the insights and experience of individuals and organisations who have shared their time and perspectives with openness and commitment.
During a six-month consultation process, we:
- heard from people living with diabetes about their hopes and experiences through our Diabetes Lived Experience Advisory Committee and members of the 2023 Tackling Inequality Commission panel
- consulted with clinical leaders, Diabetes UK Health Professional Advisory Committee, diabetes organisations and groups working among communities at greater risk of health inequities
- engaged with charities supporting people with mental and physical disabilities
- gained input from our Tackling Inequality Advisory Group of Diabetes UK Board of Trustees invited discussion and ran a survey about the strategy at the Diabetes UK Professional Conference 2025. From these insights, we were able to develop a shared vision of a fairer future. This vision stands as a call to action for everyone working to reduce the harm caused by diabetes. It has informed our own plan for action to 2030.
Terminology
There is important difference between the concepts of equality and equity. In this document, and going forward, we have shifted our language to refer to tackling inequities and achieving equity.
- Equality is about ensuring everyone is offered the same resources and support. It assumes that treating everyone the same will lead to fair outcomes.
- Equity recognises that for some groups of people there are greater barriers to access and opportunity and that additional, distinct and focused resources may be needed to achieve the desired outcome.
Equity, diversity, and inclusion (EDI)
We recognise that tackling health inequities must start from within Diabetes UK and the wider professional diabetes community.
This strategy lays out how we will embed EDI in our work and our organisation, so we are representative and tuned-in to the lived experiences of everyone affected by diabetes in the UK. We have already made progress in this area, but we have more to do to create a truly inclusive culture.
Increasing diversity within the diabetes healthcare and research community is also essential. A more diverse workforce fosters greater trust and engagement, and supports culturally competent care and research activity that reflects the realities of the communities we serve.
External priorities
Health inequities negatively impact many different communities. Tailored and targeted work is needed to understand the root causes and find effective solutions with every group.
We will focus first with Bangladeshi, Pakistani, Black African and Black Caribbean communities, as well as those experiencing poverty.
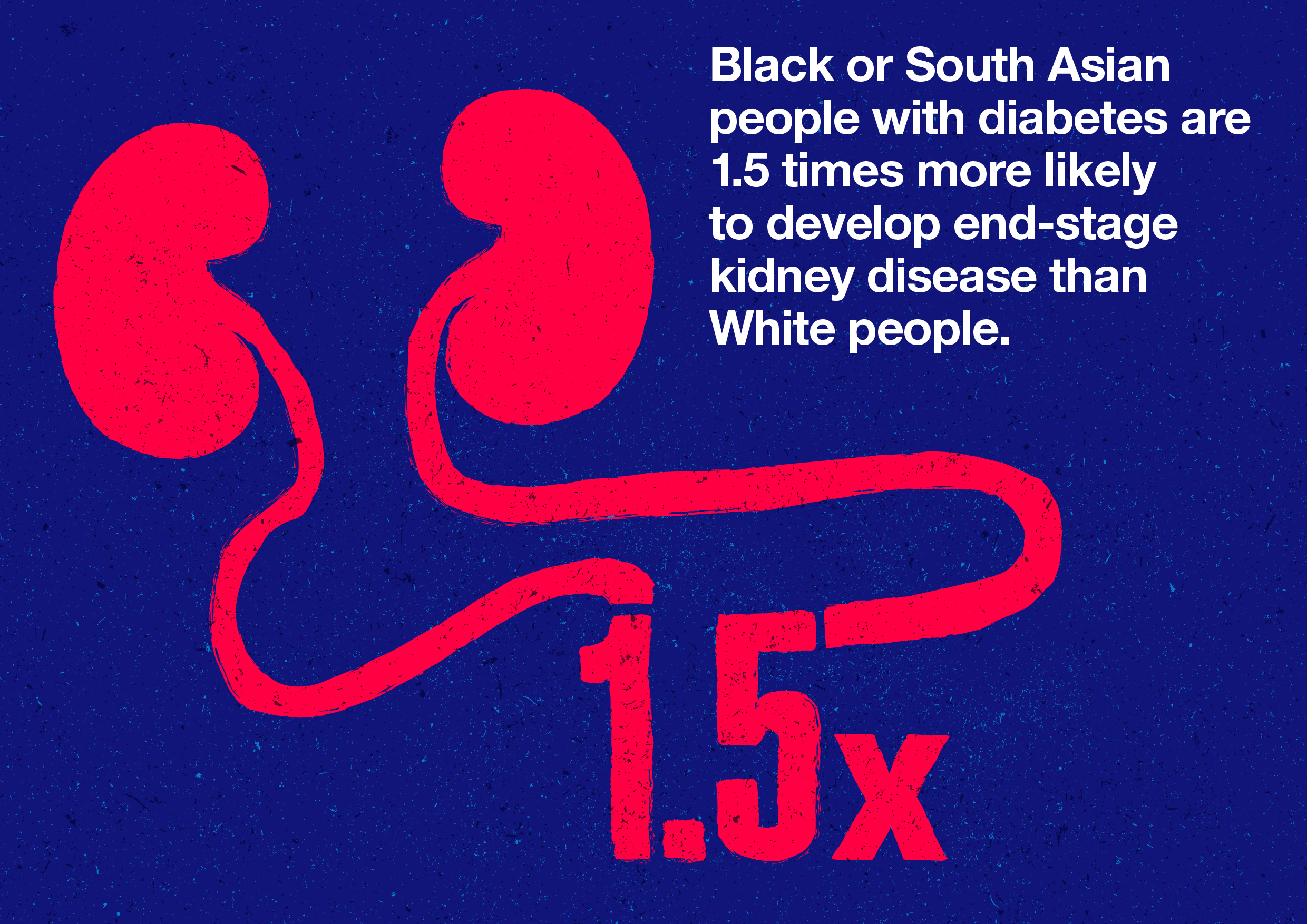
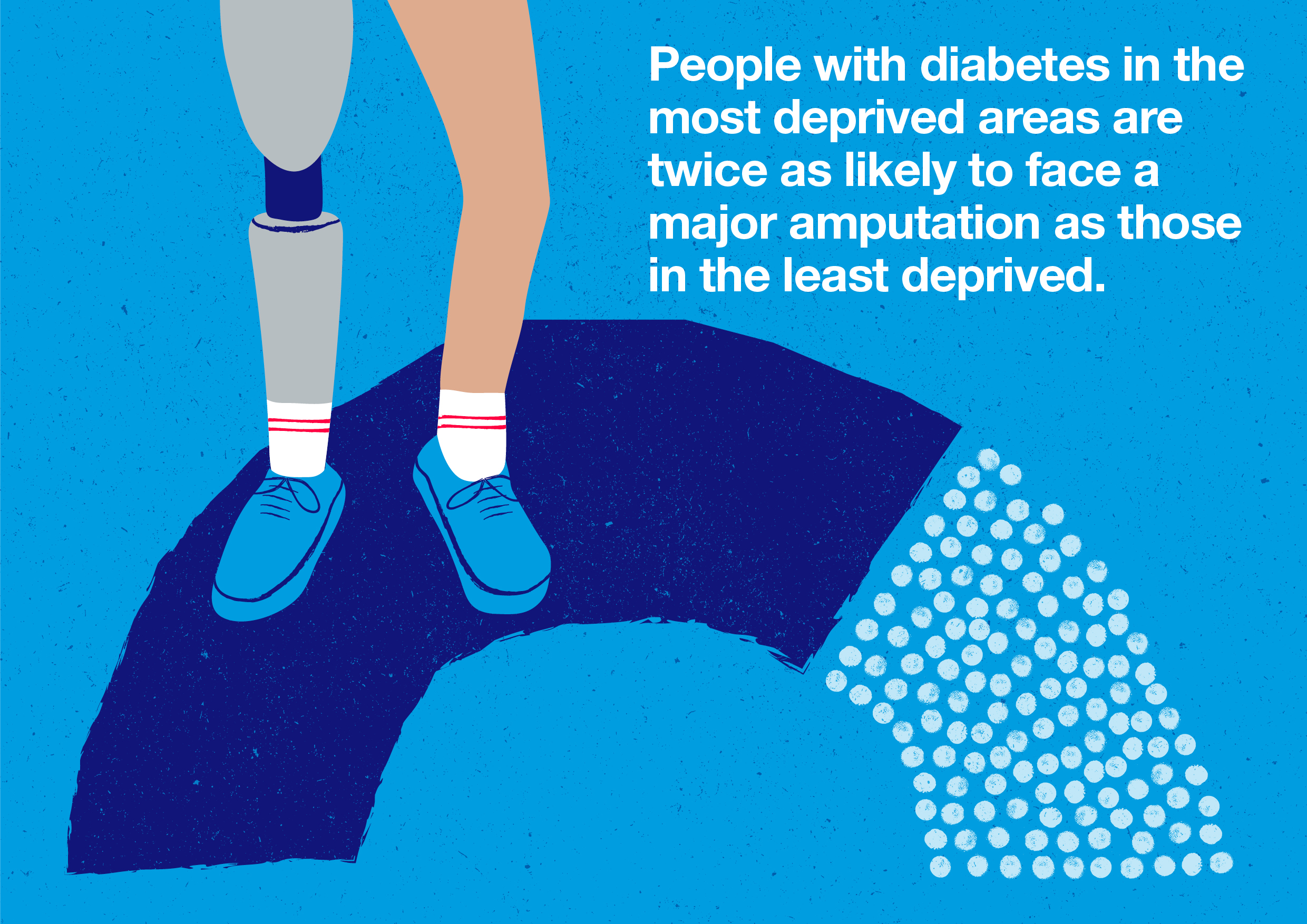
These groups are at a disproportionately high risk of developing type 2 and gestational diabetes, as well as facing inequities in access to care and treatments across all types of diabetes, which worsens outcomes. Factors like disability, gender and postcode intersect with these ethnic and economic status to further deepen disparities.
A robust approach
We will use quantitative and qualitative data and insights to drive decisions, work with others to address systemic barriers (such as systemic racism), and diversify ourselves and the healthcare and research landscape to create lasting change.
Colette Marshall, CEO at Diabetes UK, said:
Millions of people in the UK are living with diabetes [iv]. It is a serious condition made more severe by the effects of deep-rooted inequities experienced by some communities.
Despite recent progress in closing some gaps in care and widening access to diabetes technology, diabetes inequity in other areas has grown. People from global majority communities, people in poverty, and people in other vulnerable groups still face a disproportionately high risk of developing type 2 diabetes, poorer access to treatment and the harshest consequences of diabetes, often without full access to the care, technology, and support they need.
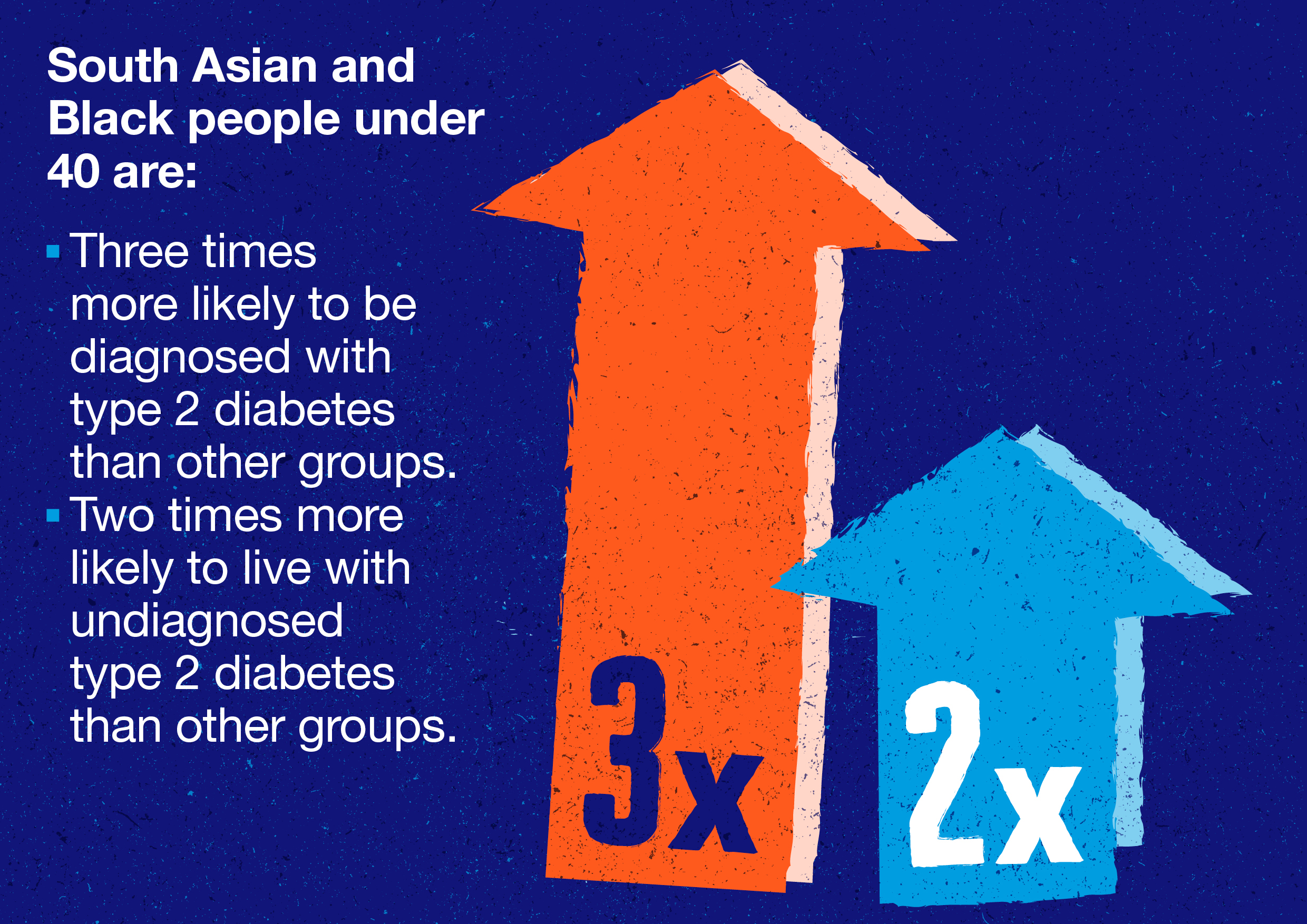
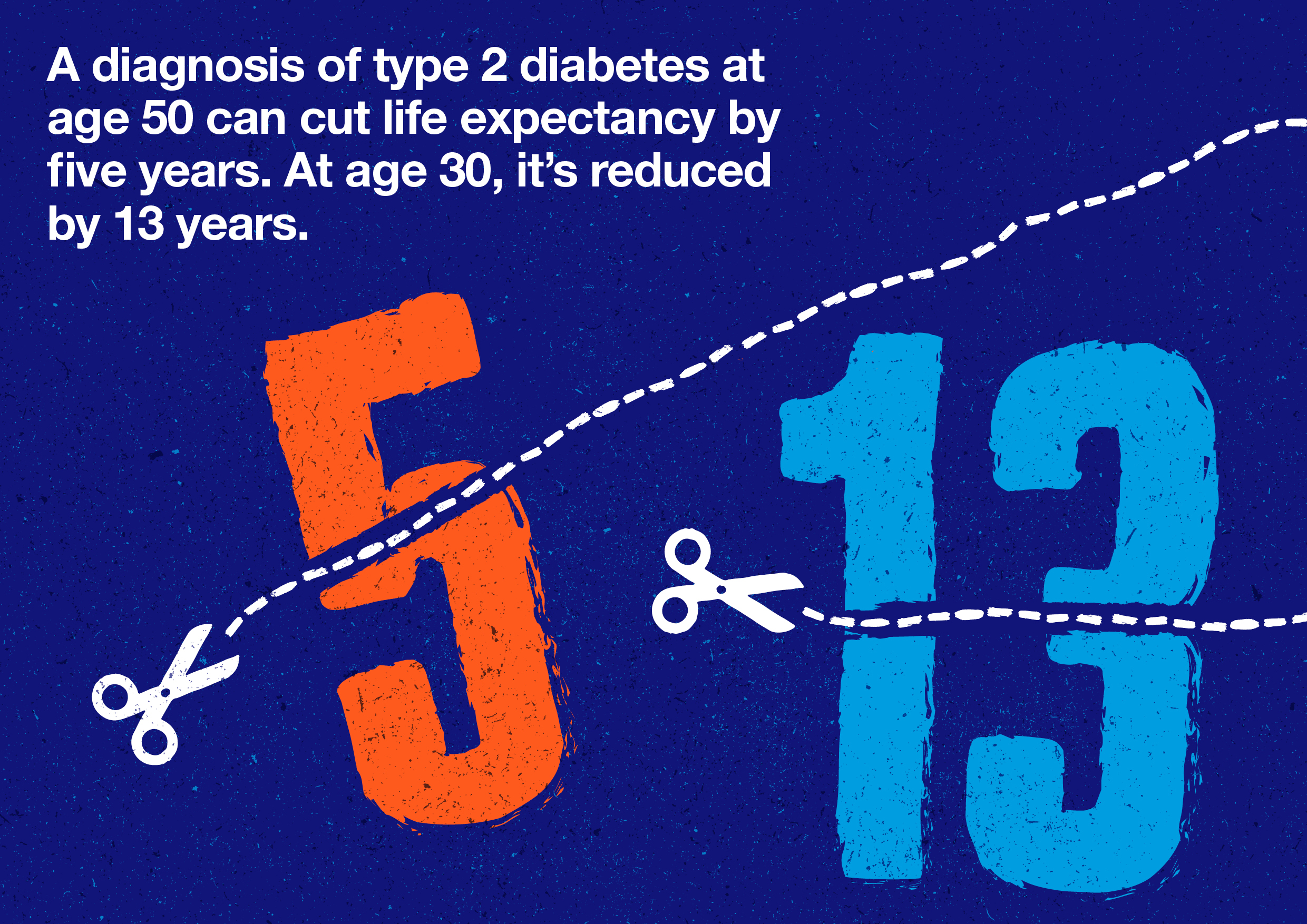
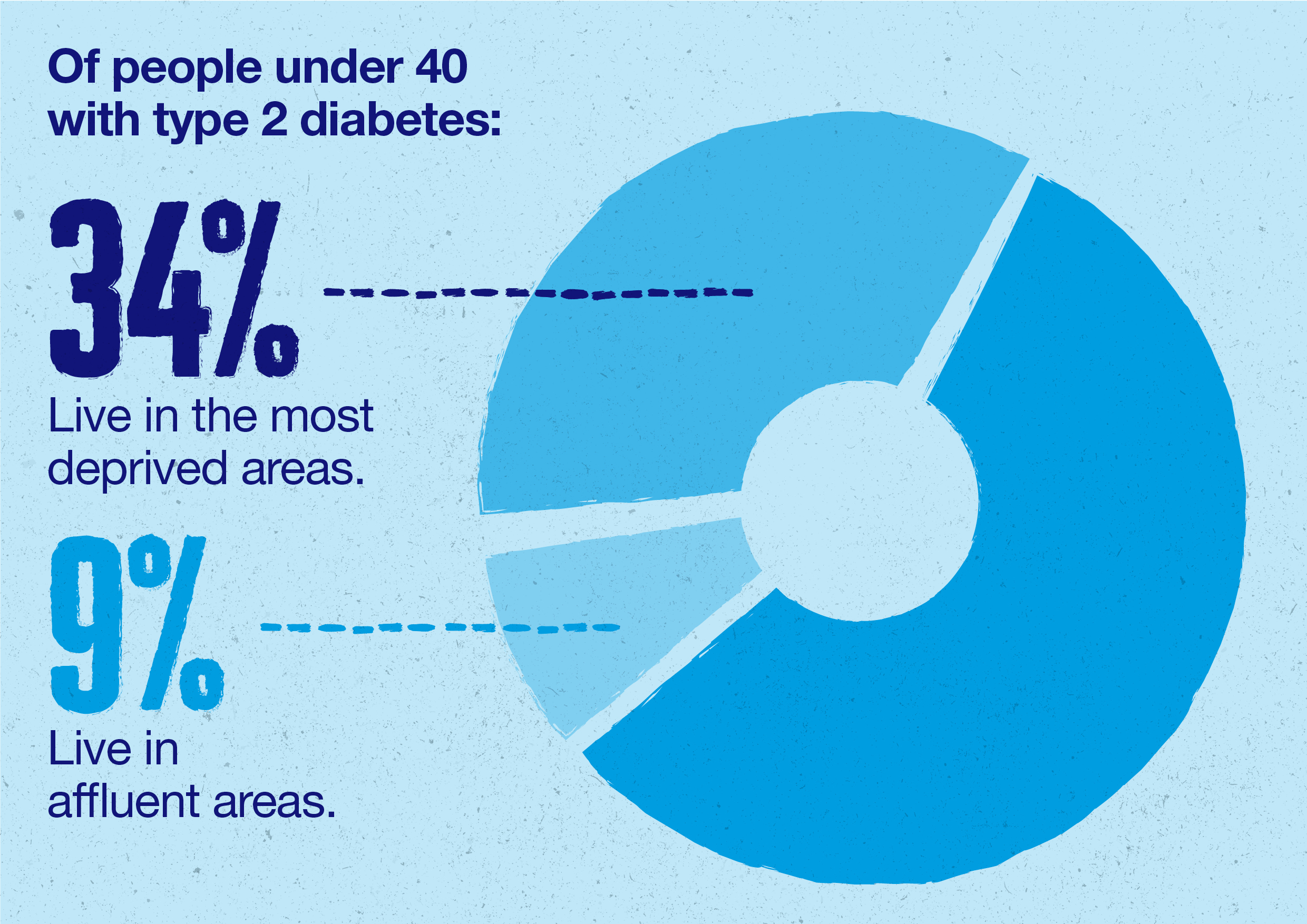
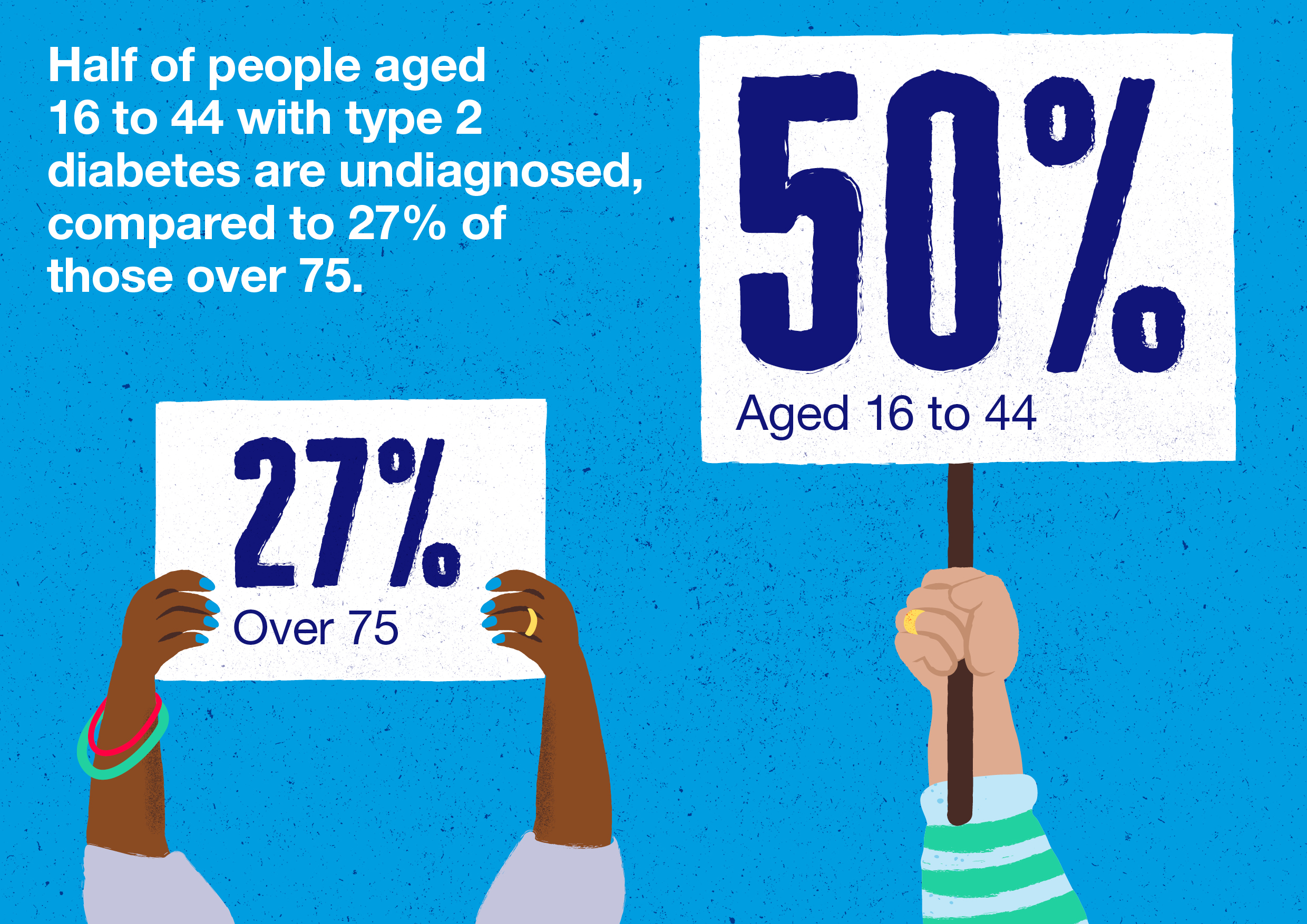
The current alarming increase in type 2 diabetes in the under-40s in the UK is being experienced more by people from Black and South Asian ethnic backgrounds and those in deprived areas. People in these communities are up to four times more likely to develop type 2 before 40 than others [v]. This unequal burden is a consequence of wide-ranging systemic inequities such as worse access to healthcare, poor housing, insecure work and barriers to accessing healthy food [vi].
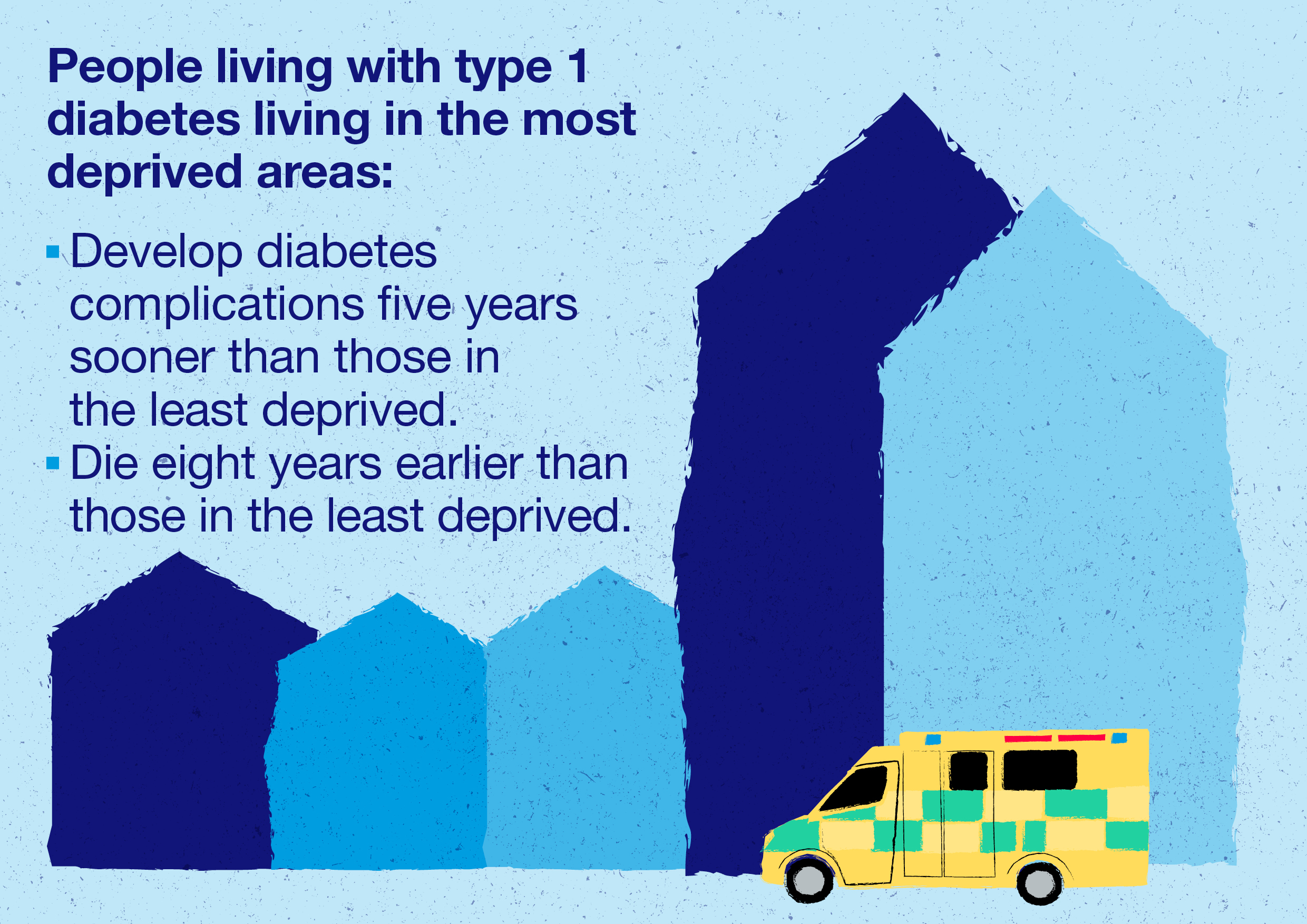
People with type 1 diabetes who live in the most deprived areas develop complications earlier and have shorter life expectancy than those in less deprived areas. This disparity remains even after accounting for health risk factors, showing that socioeconomic deprivation is an independent contributor to lives being cut short by type 1 [vii].
Tackling such inequities remains one of Diabetes UK’s most pressing priorities and here, for the first time, we present a dedicated five-year strategy for our work in this area. This document unites our actions to challenge unfairness across the UK with work to improve our own Equity, Diversity, and Inclusion (EDI). Incorporating this internal focus is crucial for our ability to be truly effective in this space and to serve the UK’s diverse diabetes population.
Whether it's early detection or providing equitable access to advanced treatments and technologies, we'll push for tailored solutions that meet the unique needs of different groups, recognising the need to take an intersectional approach. We know that overlapping factors like ethnicity, socioeconomic status and structural disadvantage combine to deepen disparities and we must make sure that our and others’ efforts in prevention and care are embedded in these realities. We’ll also continue our work to address diabetes stigma, which creates barriers to care and impacts disadvantaged groups the most.
Partnership, collaboration and influence across sectors is crucial for equitable progress, and we’ll seek out opportunities to amplify and add our voice to the efforts of others. We’ll work closely with trusted community organisations and leaders at every stage, to co-produce solutions with the communities most affected.
We invite you to work with us and help make a real impact—we need funding, resources and voices in support of fighting unfairness. This is not a quick fix, but together we can create a better future for everyone living with or at risk of diabetes, ensuring no one is left behind.
Acknowledgements
We are grateful to everyone who engaged with the development and consultation processes that informed this strategy, including the following groups, organisations and individuals.
Advisory Group of Diabetes UK Board of Trustees:
- Dr Sarah Ali - Consultant in Diabetes and Endocrinology at Royal Free London. Clinical Lead for the Barnet Diabetes Integrated Service
- Professor Linda Bauld - Bruce and John Usher Chair in Public Health, University of Edinburgh and Chief Social Policy Adviser, Scottish Government
- Michael Gibbs – Crisis Management and Transformation Specialist, Northern Ireland
- Professor Wasim Hanif - Professor of Diabetes & Endocrinology, Consultant Physician, and Head of Service in Diabetes at University Hospital Birmingham
- Melanie Stephenson-Gray - Diabetes Prevention Programme Lead, Cardiff and Vale University Health Board
- Dr Asiya Yunus – GP and Medical Director, London wide Local Medical Committees
Diabetes UK Lived Experience Advisory Committee
Diabetes UK Healthcare Professional Advisory Committee
Diabetes UK Research Steering Groups
Experts by experience:
- Arbah Azhar
- Allan McMillan
- Daniel Newman
- Nana Ocran
- Berni Warren
We are also grateful to the following organisations and individuals who have helped us to ensure this document reflects the broader barriers to equity faced by people living with diabetes:
- National Voices
- Dr Julia Platts, National Clinical Lead for Diabetes in Wales
- Dr David Blane, Academic Lead, GPs at the Deep End, Glasgow
- Thomas Pocklington Trust – National Sight Loss Charity
- Rethink Mental Illness
- RNID - National Hearing Loss Charity
- Race Equality Foundation
References
[i] Diabetes UK. (n.d.). Our strategy: A generation to end the harm, https://www.diabetes.org.uk/about-us/about-the-charity/our-strategy
[ii] Chan, J., Blane, D., Choudhary, P., Chowdhury, T. A., Goyal, A., Hanif, W., Jacca, J., Mathur, R., Misra, S., Ocran, N., Rutter, M. K., Studley, R., Treweek, S., Valabhji, J., & Khunti, K. (2023). Addressing health inequalities in diabetes through research: Recommendations from Diabetes UK's 2022 health inequalities in diabetes workshop. Diabetic Medicine, 40(6), e15024. https://doi.org/10.1111/dme.15024
[iii] Diabetes UK (2023). Tackling Inequality Commission Report.
[iv] Dabetes UK (2025) 'One in five adults now live with diabetes or prediabetes in the UK,' Diabetes UK. https://www.diabetes.org.uk/about-us/news-and-views/one-five-adults-now….
[v] National Diabetes Audit 2021-22, Young People with Type 2 Diabetes (England and Wales)
[vi] Agardh E and others. Type 2 diabetes incidence and socio-economic position: a systematic review and meta-analysis. International Journal of Epidemiology 2011. 40(3): p. 804-818
[vii] Hohn A, McGurnaghan SJ, Caparrotta TM et al (2022). Large socioeconomic gap in period life expectancy and life years spent with complications of diabetes in the Scottish population with type 1 diabetes, 2013-2018. PLoS One 17 (8). doi: 10.1371/journal.pone.0271110













