
Why's it good to move?
You’re definitely not sweating the small stuff when it comes to exercise and Type 2 diabetes...
There are many vitally important reasons to make physical activity a regular part of your lifestyle. As well as helping to maintain healthy blood sugar levels, exercise can play a key role in your overall health, as you will find out.
If you could be exercising more, we hope that this information will help you to do so safely, and in accordance with advice from your diabetes team.
Sports nutrition and type 2 diabetes
What's the difference between physical activity and exercise?
The terms ‘physical activity’ and ‘exercise’ are often used interchangeably, although there is a small difference: physical activity includes all movement that increases energy use (or calories burned) e.g. housework and gardening. On the other hand, exercise refers only to structured exercise e.g. running or lifting weights.
Why bother distinguishing between the two? For optimal health, only focusing on structured exercise isn’t ideal.
What are the benefits of exercise?
- Improved blood glucose. An interesting fact, exercising muscles use 7–20 times more glucose than non-exercising muscles
- Improved cardiovascular health. E.g. lower blood pressure and triglycerides, and increased beneficial HDL cholesterol
- Contribution to weight loss. Exercise is especially beneficial for keeping weight off for those who have lost weight
- Improved quality of sleep (but likely not if exercise is performed too close to bedtime)
- Beneficial for cognitive (brain) function and health
- Reduced stress hormones
- Better mood and outlook
- Improved self-confidence.
Other benefits of exercise include reduced stress hormones, better mood and outlook and improved self confidence.

Exercise and type 2 diabetes
A study where researchers told people with type 2 diabetes to "take a short walk right after meals" proved the advice to be a very good exercise prescription.
Results from the study showed that blood glucose levels after meals dropped an average of 12 per cent when people walked for only 10 minutes after three daily meals, compared with walking for 30 minutes at any time of day.
The biggest effect was a 22 per cent drop in blood glucose in the 3 hours after the evening meal.
One specific area of health where exercise is proving beneficial, is cognitive brain function. With Alzheimer’s disease statistics growing, concerns about healthy brain ageing are coming to the forefront.
Evidence indicates that Alzheimer’s disease, and mild cognitive impairment, are disorders of insulin resistance (similar to type 2 diabetes).
So, any intervention that increases insulin sensitivity may have the added effect of protecting cognitive function. In particular, exercise aimed at increasing and/or preserving muscle mass may be especially beneficial for facilitating healthy brain ageing.
Since muscle mass declines as we age, we have to be mindful of the types of exercise we do, as outlined below.
Defining exercise intensity
Are you working hard enough during your exercise sessions?
To achieve your individual goals – both physically and in terms of your diabetes management – it's important to know that the exercise you are doing is in line with those aspirations.
Below is a specific definition of intensity that's based on your perceived effort:
- Moderate intensity: 50–70 per cent of maximum exercise effort
- Vigorous intensity: 70–90 per cent of maximum exercise effort
- Highest intensity: 90–100 per cent of maximum exercise effort
Types of exercise and physical activity
It’s useful to have an understanding of the different types of physical activity and exercise. Types of exercise include:
- Aerobic exercise: This includes activities such as walking, cycling, jogging and swimming performed at a steady intensity.
- 'HIIT; exercise (a type of aerobic exercise): HIIT is an acronym for high-intensity interval training. With HIIT training, low-to-moderate intensity intervals are alternated with high-intensity intervals and can be applied to various types of aerobic exercises such as running or cycling.
- Resistance exercise: This consists of lifting free weights, using weight machines, performing exercises using resistance bands and the body’s own weight.
- Balance and flexibility exercises: Examples of this include yoga and tai chi.
For diabetes, greater health benefits are gained from doing a combination of aerobic (or high intensity interval training) and resistance exercise.
A word on HIIT
 HIIT training can be a very effective use of time and is increasingly popular, but it may not be safe for those who have diabetes complications or other health-related complications.
HIIT training can be a very effective use of time and is increasingly popular, but it may not be safe for those who have diabetes complications or other health-related complications.
If in doubt, speak to your diabetes care team.
Joint mobility may be affected by having high blood glucose, therefore including some form of flexibility work in your weekly exercise routine may also be very beneficial.
Let’s talk briefly about standing and sitting. It’s been shown that sitting for long periods can impair metabolic function.
In particular, too much sitting can lead to a decrease in the activity of an enzyme called lipoprotein lipase, or LPL, which is associated with higher triglycerides, lower levels of HDL, and an increased risk of heart disease. Sitting reduces insulin sensitivity and weakens bone density.
Non-exercise physical activity in the form of standing leads to a 2.5-fold increase in calories burned compared to sitting – employees who stand while they work burn up to 75 per cent more calories per day than those who sit all day.
As such, we need to prioritise increased movement throughout the day.
How much exercise is enough?
While any exercise is certainly better than no exercise, striving to achieve the recommendations, if able to do so, will allow you get the most health gains from a regular exercise routine.
The national guidelines on physical activity and exercise for adults are:
- Aim to be active daily. Over a week, activity should add up to at least 150 minutes (2.5 hours) of moderate intensity activity in bouts of 10 minutes or more – one way to approach this is to do 30 minutes on at least 5 days a week. For example, a brisk 30 minute walk and/or lap swimming for 5 days a week.
- Alternatively, comparable benefits can be achieved through 75 minutes of vigorous intensity activity spread across the week, or combinations of moderate and vigorous intensity activity. Before beginning a vigorous exercise routine, speak to your GP or diabetes care team.
- Aim to do physical activity which improves muscle strength on at least two days per week. For example, perform an exercise routine in the gym where you use resistance exercise machines, or do body weight exercises such as pushups and wall squats.
- Aim to minimise the amount of time spent being sedentary (sitting) for long periods. American diabetes guidelines, in particular, state that people with diabetes should interrupt prolonged bouts of sitting with bouts of light activity every 30 minutes.
How do these guidelines benefit diabetes?
- Daily exercise, or ensuring that two days do not elapse between exercise sessions, ensures that you remain insulin sensitive. The insulin sensitivity benefits of exercise wear off after about 24 hours (this is based on a person with type 2 diabetes engaging in low-intensity exercise for approximately an hour per day).
- Exercise which improves muscle mass – such as resistance exercise – is important for maintaining or building muscle as it helps the body to be more insulin sensitive. And, as we lose muscle mass as we age, incorporating some form of resistance exercise at least twice per week on non-consecutive days becomes extremely important.
When is the best time to exercise?
 The best time to do structured exercise is when you’re most likely to do it! Some find it useful to exercise first thing in the morning, while other prefer to exercise at the end of the day. Be mindful that exercising too close to bed may affect sleep quality.
The best time to do structured exercise is when you’re most likely to do it! Some find it useful to exercise first thing in the morning, while other prefer to exercise at the end of the day. Be mindful that exercising too close to bed may affect sleep quality.
If you struggle to include exercise in your day, you may find it helpful to schedule exercise into a diary, sign up for a weekly class or find an exercise partner. Being intentional with the timing of non-exercise physical activity throughout the day can go a long way to lowering blood glucose.
Therefore, aim to:
- Walk for 10 minutes or longer soon after finishing a meal
- Interrupt prolonged periods of sitting with bouts of very light activity every 30 minutes. This can mean doing a few stretches or chair-based exercises at your desk or going for a walk to get a drink of water.
We also need to look for opportunities throughout the day to make us move more in general. Here are some ideas to promote movement throughout the day:
- take the stairs instead of lift or escalator
- stand when speaking on your phone
- use a standing desk
- if possible, walk or cycle to work
- park further away from the shop’s entrance
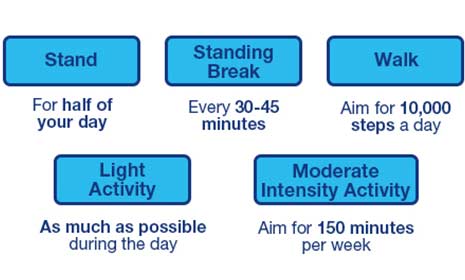
Exercise ideas by numbers:
- Stand: for half of your day
- Take a standing break: every 30–45 minutes
- Walk: aim for 10,000 steps a day
- Light activity: as much as possible during the day
- Moderate intensity activity: aim for 150 minutes per week
Preparing to exercise safely
There are several things to bear in mind if you are beginning a new exercise routine.

Medication
The concern of blood glucose going low during exercise may be on your mind.
In reality, most of the diabetes medication used by people with type 2 diabetes tends not to cause hypoglycaemia. Diabetes medication which requires extra caution is insulin and a class of drugs called insulin secretagogues.
Common examples of this include Gliclazide, Glimepiride and Repaglinide. These medications can cause hypoglycaemia during and after exercise (up to 24 hours after an exercise bout).
Insulin and exercise
Strategies to prevent hypoglycaemia if using fast-acting insulin:
- If exercising within two hours of a meal where fast-acting insulin was taken, you may need to consider lowering the insulin dose. However, monitor the effects of exercise on your blood glucose and speak to your diabetes team for advice on appropriate insulin reduction, if this is necessary.
- If exercising before a meal (e.g. exercise before breakfast) then consider reducing the fast-acting insulin dose at the meal eaten after exercise (in this case, breakfast).
If you use tablets such as Gliclazide and have experienced hypoglycaemia during exercise, have a discussion with your diabetes team as it may be an option to decrease the medication dose on exercise days.
Blood glucose
If you take medication which has the risk of causing hypoglycaemia during exercise (i.e. insulin and insulin secretagogues) it’s a good idea to check your blood glucose before exercise and, possibly, also during or after exercise.
If taking one or both of these medications and blood glucose is below 5mmol/L at the start of exercise, consider having a small carbohydrate-containing snack which contains 15–30g of fast-acting carbohydrate.
This may be similar to what you use to treat a hypo – for example, dextrose tablets or fruit juice. Remember, fast-acting carbohydrate is only required if there is a risk of your blood glucose going low (below 4 mmol/l). Do not take fast-acting carbohydrate just ‘in case’ – instead, always carry a source of glucose with you whilst exercising.
If blood glucose is high (greater than 14 mmol/l) before exercise, there may be the risk of your blood glucose continuing to rise because you do not have enough circulating insulin. In this instance, avoid high-intensity, vigorous exercise and, instead, perform more gentle, lower-intensity exercise.
Do you have diabetes complications?
If the answer is yes, you may want to consider the following:
Nerve disease
- Use suitable footwear
- Do mostly non-weight bearing activities, especially if gait is altered or if foot deformity is present
- If you have foot ulcers, avoid weight bearing activity, including jogging
- If you have postural hypotension, avoid activities with rapid changes in direction to avoid falling or fainting
Eye disease
- If you have moderate or severe non-proliferative retinopathy, avoid activities that dramatically raise blood pressures, such as weight lifting
- With severe non-proliferative retinopathy, avoid all kinds of vigorous activity, jumping and breath holding
Kidney disease
- If microalbuminuria is present, most activities are safe, but avoid vigorous exercise the day before urine protein tests
With overt nephropathy (and if on dialysis), it's best to avoid high-intensity and strenuous exercise.
 Fuel your exercise
Fuel your exercise
An understanding of what to eat – and what to avoid – whilst exercising is central to your success. Although true of all people, if you are living with type 2 diabetes it can be even more important.
The information below offers some useful starting pointers and may answer some initial questions about type 2 diabetes and sports nutrition. However, if you require more detailed information, and even the development of an appropriate meal plan, always speak to your diabetes team.
No matter what exercise or physical activity you are taking part in, give yourself the best start diet-wise and fuel yourself for maximum performance.
- Sports nutrition products such as energy drinks and gels are a very convenient source of fast-acting carbohydrate when performing moderate- to high-intensity exercise and long-duration exercise such as marathon running. These products must be used strategically – unless absolutely required for exercise performance or to prevent hypoglycaemia, they are best avoided.
- For long-duration, but low-intensity exercise such as hiking, and if you are not at risk of hypoglycaemia, there is also no need to consume sports nutrition products such energy gels and sports drinks. Instead, choose whole foods such as bananas or other fruits and nuts if you wish to eat something.
- Stay well hydrated. In most cases, water is adequate, although you can also consider having sugar-free electrolyte drinks. Increasing your fluid intake is especially important if you exercise with high blood glucose levels.
- Protein is an important nutrient for building muscle or maintaining muscle mass. Where possible, rely on whole foods to obtain your protein. Protein-rich foods include meat, fish, chicken, eggs and dairy foods – quark, cottage cheese and Greek yogurt are particularly high in protein. Vegetarian sources of protein include pulses, nuts and seeds. Ensure you have some protein at each meal, including breakfast.
