There isn’t a cure for diabetes right now.
But our scientists across the UK are pushing boundaries and taking steps to build a future where diabetes can do no harm. Here are some of the ways we’re trying to achieve this goal for both Type 1 and Type 2.
Type 1 diabetes
Type 2 diabetes
Type 1 diabetes
In Type 1 diabetes, insulin-producing beta cells in the pancreas are destroyed by the immune system. This means you can’t make the insulin you need to live.
We've linked up with the Steve Morgan Foundation and JDRF to accelerate the development of new treatments and a a cure for type 1 diabetes. Find out more about the Type 1 Diabetes Grand Challenge.
Stopping the immune attack

To stop Type 1 diabetes we need to disrupt the immune system’s attack on beta cells. And our scientists are working on it. They’re aiming to develop and test treatments – called immunotherapies – that target the immune system to stop it destroying beta cells.
This means in the future we could stop people from ever developing Type 1 diabetes.
In people who are at high risk of getting Type 1 diabetes, immunotherapies tested in trials have been able to delay the onset of the condition for a few months. Scientists are now exploring whether giving treatments earlier on, in younger children, could have better success at preventing Type 1 entirely.
Immunotherapies also have potential to help people newly diagnosed with Type 1 diabetes. Researchers hope to be able to slow down or halt the immune attack to protect surviving beta cells. And it seems they might be able to, at least in the short-term. Treatments that have been tested so far can preserve the amount of insulin people make and improve their blood glucose control. But the protective effects appear to dwindle over time.
Work is now being done to look at how we can combine immunotherapies to target different parts of the immune system, and have a greater impact.
Find out more about how immunotherapies work and our research in this area.
Beta cell replacement
For people already living with Type 1 diabetes, a cure is likely to mean a combination of different treatments.
First, we need to replace the beta cells that have been destroyed by the immune system, so people with Type 1 diabetes can make enough of their own insulin again.
Transplants using cells taken from donors already exist. But they stop working over time and there are a limited number of donated pancreases available. So scientists are trying to make an unlimited supply of beta cells in the lab.
Lab-made cells have already been implanted into animals and shown to successfully treat their Type 1 diabetes, but we don’t know how lasting the benefits are.
More recently, researchers in Canada and USA moved into testing the transplants in people with Type 1 diabetes. They’ve shown transplants are safe, and trials are underway right now to see if they can improve the amount of insulin people with Type 1 diabetes make. This is a really exciting milestone, but there’s still a way to go before this kind of treatment could be used to replace insulin injections or pumps.
But we’re funding research to get us there quicker. Dr Natasha Hill is hoping to make fully working beta cells from stem cells and then see if they can successfully treat Type 1 diabetes in mice.
Beta cell protection
Next up, we need to protect the newly transplanted beta cells from being destroyed by the immune system. One way to do this may be through immunotherapies, which aim to retrain the immune system so it won’t attack the pancreas.
Another potential route is to transplant beta cells in a protective barrier. This is called beta cell encapsulation. This barrier would allow beta cells to sense blood glucose levels and let important nutrients they need to survive in, but would block rogue immune cells from attacking.
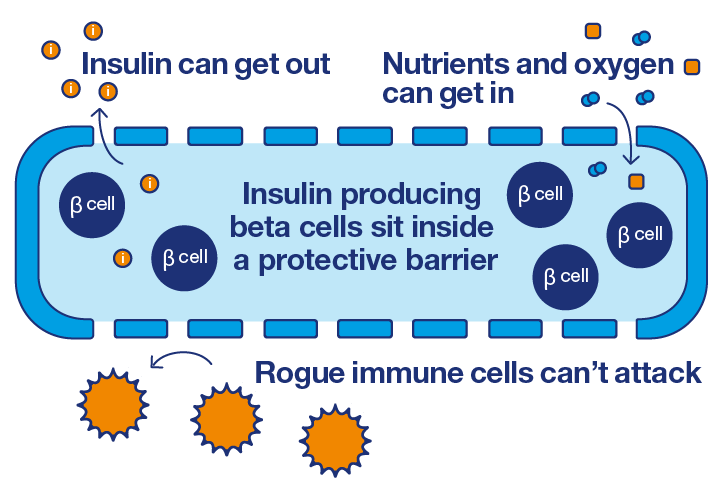
Different methods of beta cell encapsulation have been tested in animals and shown to successfully protect cells for up to six months. A handful of encapsulation devices have also been tested in trials with people with Type 1 diabetes – showing they’re safe in the short-term. Researchers are now beginning to test if they can protect against immune destruction and help to control blood glucose levels.
This is a really encouraging and fast growing area, but there are still barriers to overcome. Scientists need to test if protective devices are safe and beneficial for the longer term. And work out how to make these treatments accessible and less expensive.
Type 2 diabetes
In Type 2 diabetes the body stops responding to insulin, beta cells stop working properly and they lose their ability to produce insulin over time. This means you can’t make the right amount of insulin your body needs.
Type 2 diabetes remission

A hugely promising area of research in Type 2 diabetes is now showing that remission is possible. Remission means that people have normal blood glucose levels without taking any diabetes medication.
Our scientists are breaking new ground in understanding how to put Type 2 diabetes into remission. One approach that’s showing exciting promise is weight management.
When it comes to weight loss, people can go into remission through different ways. But most recently there’s been a real buzz around the results from our DiRECT trial, which is testing a low-calorie diet alongside weight loss support from a healthcare professional. At the end of year one, just under half of people taking part in the trial were in remission.
A cure can mean different things to different people. While those who have put their Type 2 diabetes into remission may see it as a cure, it’s important to remember the condition might come back. Because of this, you’ll need to carry on having regular health checks. Remission also won’t be possible for everyone with the condition.
Excitingly, the evidence building around remission is changing the way we think about Type 2 diabetes. Thanks to our research, it’s not necessarily a lifelong condition for everyone.
Replacing beta cells
Just like in Type 1 diabetes, our research to engineer beta cells in the lab could lead to ways of replacing cells that have stopped working in people with Type 2 diabetes.
Researchers in Canada have recently shown that a combination of stem cell transplants and diabetes medication successfully treated mice with Type 2 diabetes. And there are early trials going on with people with Type 1 diabetes. If successful these could pave the way to cell replacement therapies for Type 2 diabetes as well.
Rebooting beta cells

Scientists are exploring ways to keep beta cells healthy, to stop Type 2 diabetes from progressing.
Our research fellow, Professor David Hodson, is looking at one way to do this. He’s using state-of-the-art imaging technology to find out how beta cells work together in the pancreas. In mice, he found that the pancreas starts working properly again when a small group of beta cells (called hubs) are switched on. This opens up possibilities of kick starting these hubs to help people make the right amount of insulin.
We’re also supporting Dr Leclerc, who is attempting to work out if a particular molecule (called sorcin) can protect beta cells from becoming exhausted and keep them healthy.
Research to reboot beta cells is in its early days, but it’s exciting stuff. Scientists are working in the lab to build knowledge on the biology behind beta cell failure in Type 2 diabetes and develop new ways to stop it.
Research like this is helping us create a world where diabetes can do no harm.
But our scientists across the UK aren't finished. And it’s only with your help that we can push ahead with ground-breaking research. Will you donate today and help us lead the fight against diabetes?
