In type 1 diabetes, the immune system mistakenly identifies insulin-making beta cells as a threat and sets about destroying them.
Decades of research have shown that this process doesn’t happen overnight. It begins quietly, months or years before symptoms appear. We can detect early warning signals from the immune system that show its attack is already underway.
This opens up a window to use new treatments, called immunotherapies, to calm the immune system down and delay, or even prevent, type 1 diabetes from developing.
Early warning signs
These warning signs are called islet autoantibodies - proteins designed to attach to beta cells and earmark them for destruction.
They can be detected with a simple blood test, telling us if someone is likely to develop type 1 diabetes in the future. This is known as type 1 diabetes autoantibody screening.
How can I get tested?
Right now in the UK, screening for type 1 diabetes autoantibodies is only available as part of research studies. You or your child may be eligible to take part.
- Children aged 3-13 years can sign up to the ELSA study, funded by Diabetes UK and Breakthrough T1D. ELSA will answer important questions that could help to make type 1 diabetes autoantibody screening in children a reality in the UK.
- Adults aged 18-70 years can get screened through a similar study, called T1DRA. It's looking to understand more about how type 1 diabetes develops in adults.
What does it mean if I have autoantibodies?
The immune system can make several different autoantibodies linked to type 1 diabetes. Type 1 diabetes autoantibody screening shows whether you have them, and how many.
From studies with children, researchers have learned that the more autoantibodies present, the higher the chance of developing type 1 later on. For adults, though, the picture is less clear and we still don’t know exactly how autoantibody results translate into future risk.
- You have no autoantibodies. You're not at high risk of developing type 1 diabetes. It's not a guarantee that you'll never get the condition, but we know your immune system isn't planning an attack at the moment.
- You have one autoantibody. Your risk of developing type 1 diabetes is higher than someone who has no autoantibodies – about a 15% chance over the next 10 years. However, most people with a single autoantibody won’t develop type 1 diabetes. Autoantibody numbers can increase, stay the same or decrease over time.
- You have two or more autoantibodies. This is considered early-stage type 1 diabetes. Your immune system has started attacking beta cells, but you can still produce enough insulin. The chance of progressing to full-blown type 1 diabetes within the next 15 years is around 85%. And almost 100% over your lifetime.
There are three stages of early type 1 diabetes
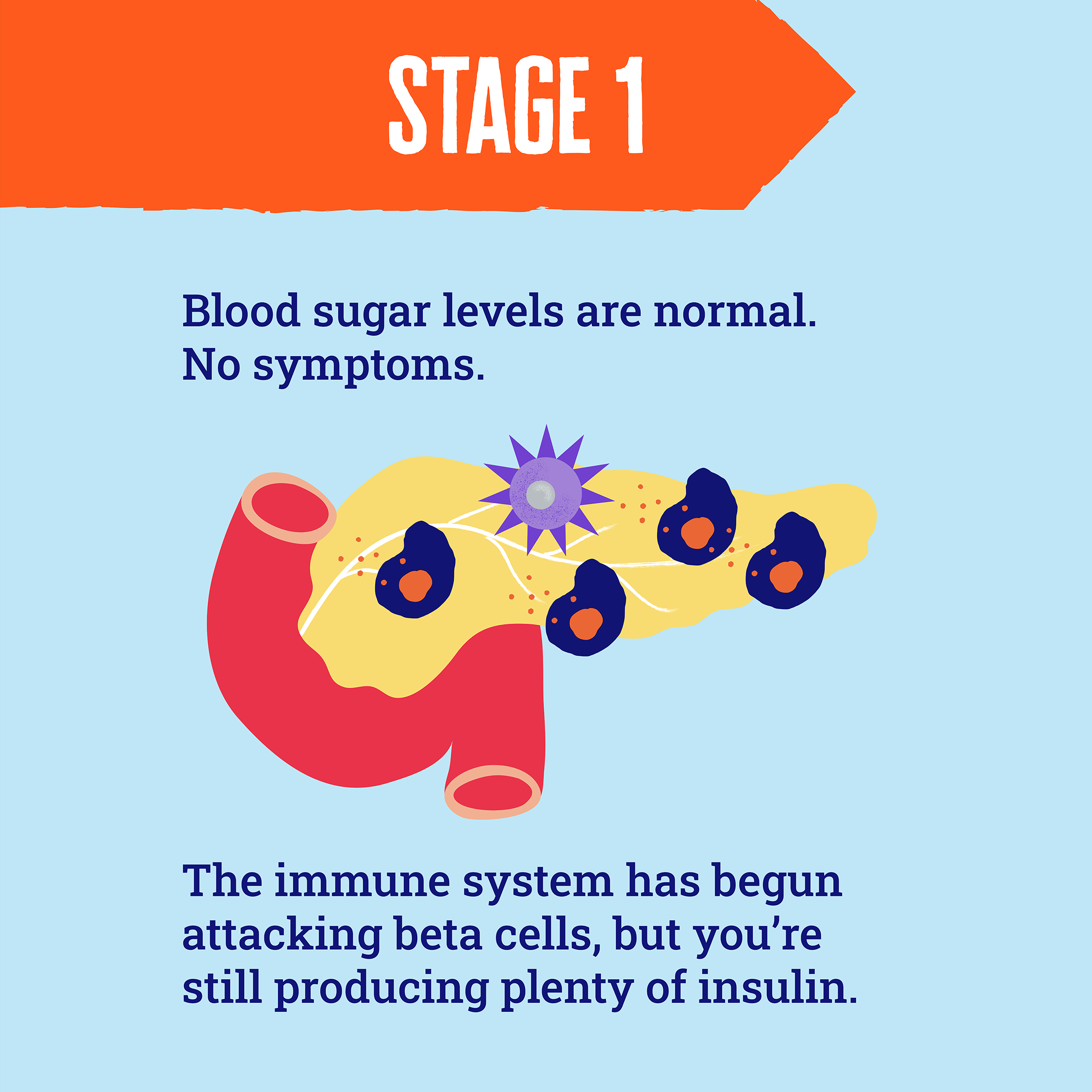
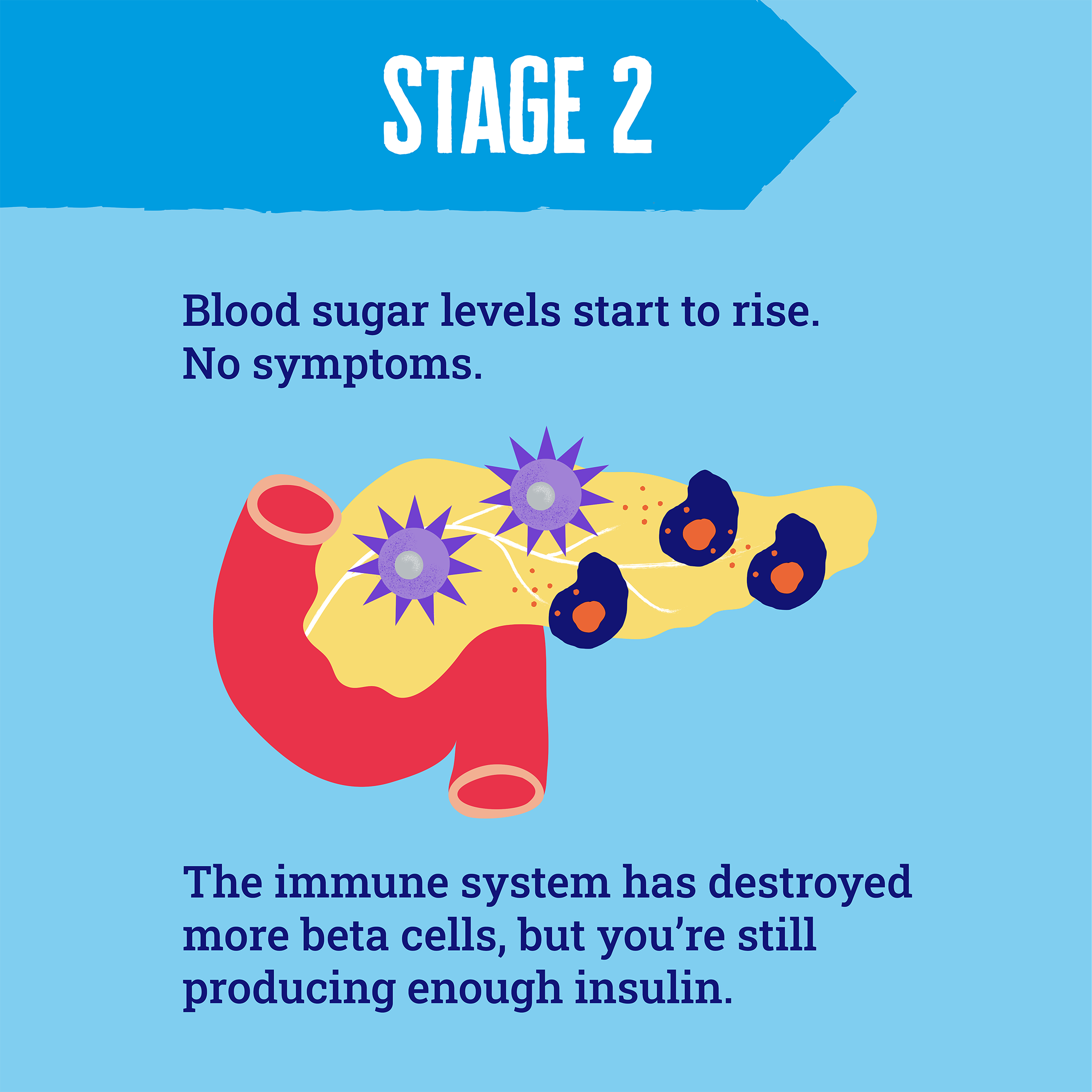
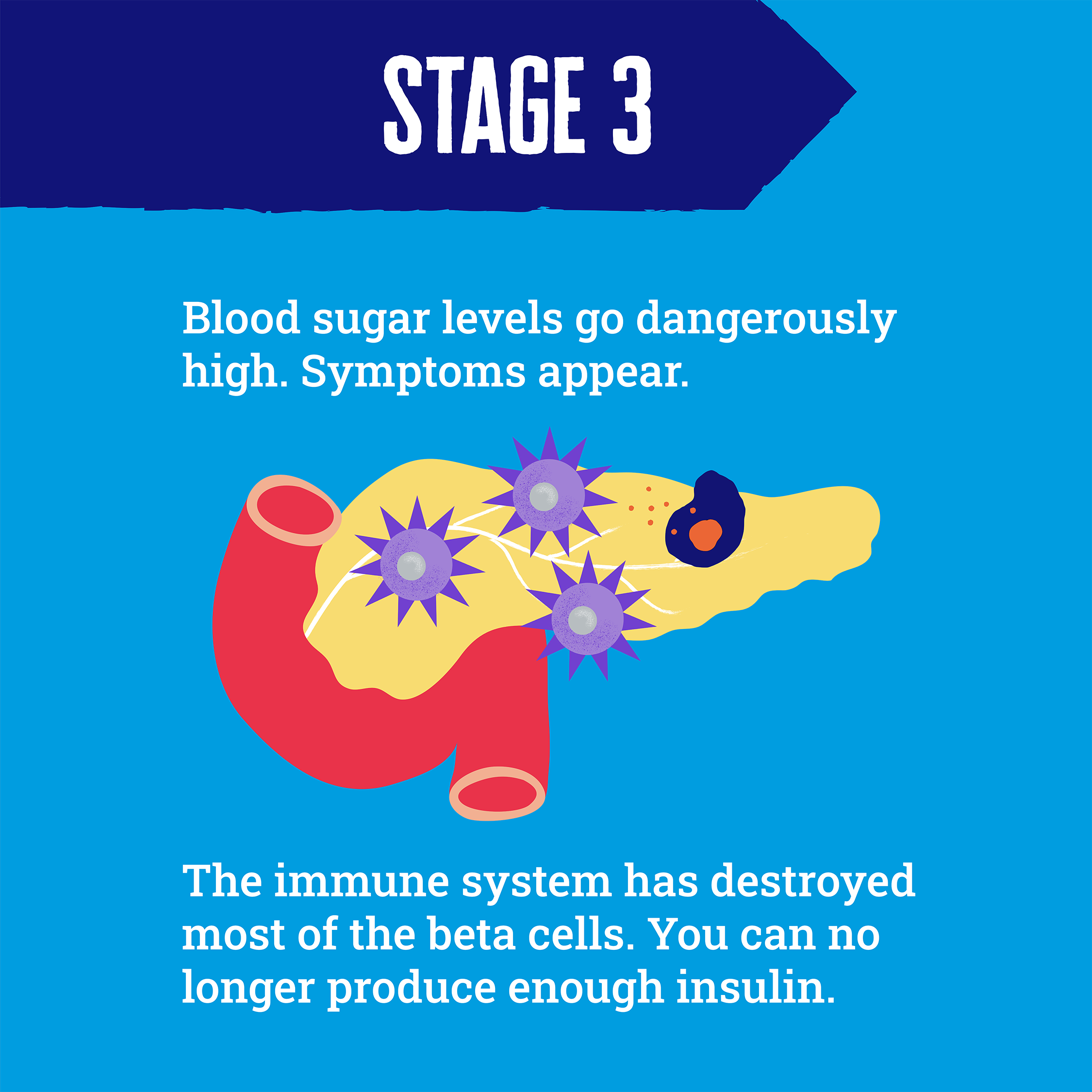
Early-stage type 1 diabetes - when two or more autoantibodies are found - is the symptomless phase before type 1 fully develops and insulin treatment is needed. This phase can last for months or years. Scientists have discovered that people progress through three distinct stages of early type 1 diabetes.
How screening could help
Autoantibody screening to detect early type 1 diabetes could make all the difference. Here are some key benefits.
Early, safe diagnosis
Around 25% of children don’t get diagnosed with type 1 diabetes until they are in potentially life-threatening diabetic ketoacidosis (DKA). Evidence shows that autoantibody screening can reduce this risk to near zero.
Screening allows healthcare professionals to closely monitor people with early type 1 diabetes and start insulin treatment sooner, before blood sugar levels become dangerously high.
Starting insulin earlier and avoiding DKA at diagnosis is linked with closer-to-target blood sugar levels years later, which can help to protect against diabetes complications.
Time to prepare
Knowing who is very likely to develop type 1 diabetes provides time for support and education to help prepare. This includes learning about insulin injections, carb counting and hypos, helping people have a ‘softer landing’ into life with type 1 diabetes.
Access to new treatments
People with early type 1 diabetes may be eligible to take part in clinical trials testing promising immunotherapy treatments, designed to halt or slow the immune system's attack.
One such immunotherapy – teplizumab (Tzield) – is licensed in the UK for people aged 8 years or over at stage 2, but isn't yet routinely available on the NHS.
We’ve been funding pivotal research to develop and test a pipeline of immunotherapies, to find more that work. In the future, we hope that people with early type 1 diabetes will have access to a selection of immunotherapies to delay, or entirely prevent, their diagnosis.
You can learn more about immunotherapies.
Getting screened for type 1 diabetes autoantibodies is a very personal choice. For some, knowing they are very likely to develop type 1 diabetes in the future can cause anxiety. That’s why it’s crucial that people identified with early-stage type 1 diabetes receive the right support.
The future of screening
The ELSA study and further research will provide vital information on whether widespread routine type 1 diabetes autoantibodies screening in the UK is practical, acceptable to people who take part and cost-effective.
We also need to work out how best to support people with early type 1 diabetes within the NHS.
That’s why we’re funding Dr Rachel Besser at the University of Oxford, who has set up the UK-Islet Antibody registry. Anyone who has tested positive for type 1 diabetes autoantibodies can register. The aims are to closely monitor people with type 1 diabetes autoantibodies, find out the best way to look after their physical and emotional health, and connect them to immunotherapy clinical trials.
We’ll continue funding research and working with key players in the NHS to pave the way for a future where we no longer wait until type 1 diabetes fully develops to diagnose and treat it.
If you’re worried about your or your child’s risk of type 1 diabetes, the most important thing you can do is be aware the signs and symptoms of the condition and to see a healthcare professional if you notice any of them.
